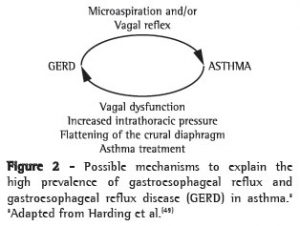
The first reference to “Esophageal Reflux as a Trigger in Asthma” was published in Chest by (Dis Chest 1966;49;464-466) in 1966. While the concept is appealing on some level from a physiologic standpoint, trials of reflux treament for severe asthmatics have been disappointing. Studies occasionally showed improved symptoms at times with anti-reflux therapy but seldom is there ever improvement in PFTs. Questions regarding long term safety of PPIs complictate this issue further. The proposed relationship between asthma and GERD may be summarized in the following image:
In my experience, some “asthmatics” responding only to high dose oral steroids in fact have reflux up into the throat or larynx. Laryngeal swelling from reflux is a form of injury and may respond to high dose steroids. This can lead a treating doctor to conclude that the patient has severe asthma. As the oral steroids are tapered, the cough and other respiratory symptoms recur. This looks may like severe asthma. If one has ruled out other pulmonary diseases, reflux needs to be considered—as a cause of symptoms mimicking asthma, not as a cause of obstructive airways. Instead of adding a PPI to all patients with severe asthma as the studies attempt to do, one should perform a diagnostic procedure for reflux, laryngoscopy or dual probe pH monitoring—or both. It’s important to note that patients with laryngopharyngeal reflux may also have a normal UGI endoscopy. More complicated yet is that reflux laryngitis can also present as vocal fold dysfunction mimicking asthma. Rhinolaryngoscopy is a simple office based procedure that can identify supraglottic swelling and aberrant vocal fold motion. A normal exam does not necessarily rule out LPR but if findings and the reflux symptom score are compatible then one may feel more confident acid reflux therapy. That can start with milder medications (known as H2 blockers— Zantac, Pepsid) alone with dietary modifications. If not effective then proton pump inhibitor therapy is the next step.